Behind the Screen report
Last modified: 5 June 2025, 10:03
Behind the Screen: Revealing the true cost of cervical cancer
In 2014 Jo’s commissioned a report via the independent think tank Demos to explore in detail the financial impact of cervical cancer, looking at its impact not just on individuals but also on the NHS and state more widely across all four UK countries.
Cervical screening does not have the take-up that it should and inmuch of the UK over the past ten years there has been a long, slow decline in screening coverage (the number of women being regularly screened). In England, after peaking at around 82 per cent in the late 1990s, rates are now hovering just above 78 per cent. Between 2012 and 2013, coverage fell from 78.6 per cent to 78.3 per cent. In Scotland, Wales and Northern Ireland, uptake is very similar.
This has serious implications for cervical cancer diagnosis rates and mortality and, subsequently, financial implications for the state, the NHS and individual women and their families. In this report Demos has looked at how raising screening coverage from its current level to 80 percent, 85 per cent or even 100 per cent would affect cancer incidence and costs, as well as what would happen if screening coverage continued to decline to 70 per cent of all eligible women. Due to having limited data for Scotland, Wales and Northern Ireland the Demos analysis on the savings to the NHS is calculated using figures across just England. However, the benefits of diagnosing and treating cervical cancer at an earlier stage would result in comparable cost savings to health authorities outside England as well.
Key financial findings from the report
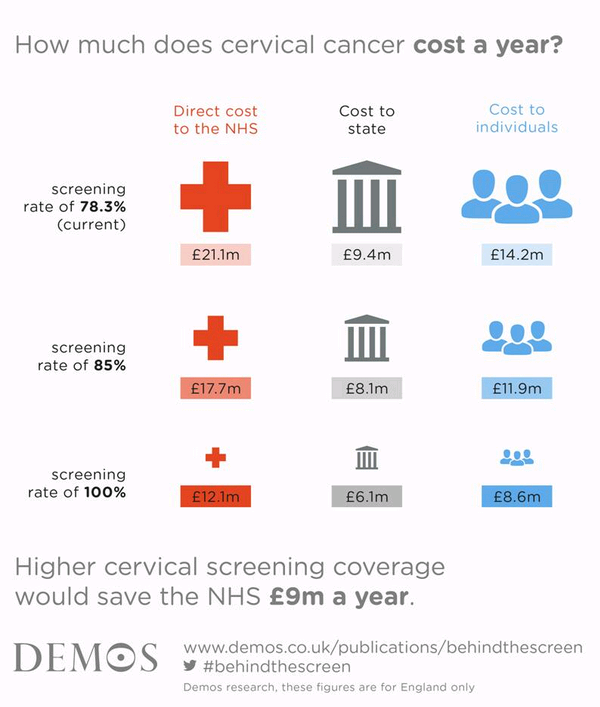
- Improving cervical screening rates would save the NHS £10m a year
- Higher rates of cervical screening would also prevent the Treasury losing up to £6m in tax revenues, and significantly ease the impact on survivors’ personal finances.
- If all women were regularly screened the annual NHS budget for cancer treatment would fall to £12.1million.
- The average cost to the NHS per person diagnosed with stage 2 or later cervical cancer is £19,261, whilst for those at stage 1a, the cost to the NHS is around £1,379 per person.The combined financial burden of cancer-related costs, additional living arrangements and loss of income for women diagnosed with more advanced cancer is £1,102 a month. However, early detection reduced the financial impact on individuals and their families to just £360 a month.
- Increased insurance premiums, special equipment and hiring extra help such as childcare or cleaners were consistently the most expensive costs to the individual.
- The majority of women also have to pay for private transport to and from appointments (66% of women), hospital parking charges (59%) and special dietary supplements or food and drink (49%).
Findings relating to incidence and mortality
England
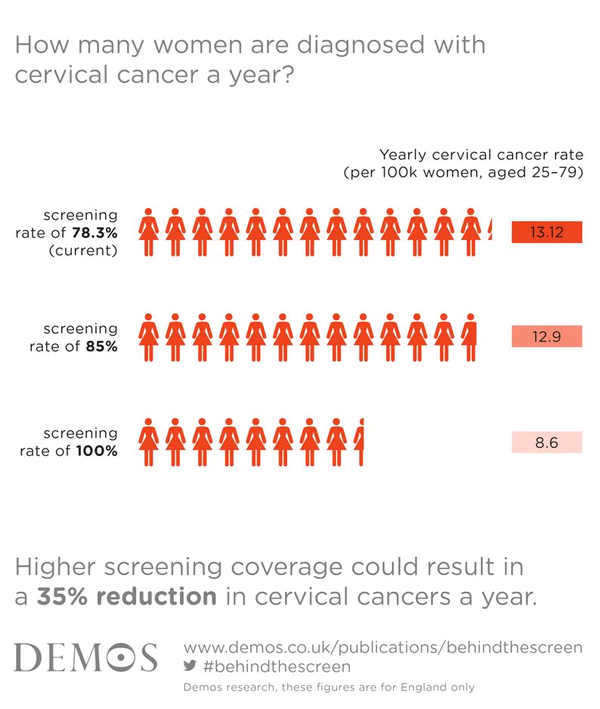
- If screening uptake rose to 85% coverage numbers diagnosed would drop by 14% in just one year and deaths would fall by 27% over five years.
- If 100% screening rate were achieved deaths from cervical cancer in England could halve and incidence would reduce by a third (35%) over five years.
Scotland
- If screening increased to 85% there would be a 21% drop in numbers diagnosed with cervical cancer in just one year and a 27% reduction in deaths over five years.
- If 100% attended annually, incidence could decrease by 41% in one year and deaths could drop by 44% over five years.
Wales
- If screening increased in Wales to 85% there would be a 22% drop in numbers diagnosed with cervical cancer in just one year and a 27% reduction in deaths over five years.
- If 100% attended annually, incidence could decrease by 41% in one year and deaths could drop by 44% over five years.
Northern Ireland
- If screening increased in Northern Ireland to 85% there would be a 23% drop in numbers diagnosed with cervical cancer in just one year and a 27% reduction in deaths over five years.
- If 100% attended annually, incidence could decrease by 39% in one year and deaths could drop by 44% over five years.
Following these findings Jo’s Cervical Cancer Trust is now looking at ways to reverse this worrying fall in screening rates across all age groups, but particularly among those who receive their first screening invitation (25-29) where one in three do not attend, and older women (50-64) who are invited every five years. Below are several recommendations from the charity on what we would like to see happen over the next couple of years:
- Gain alignment and investment at a national level for long term campaigns
- Target hard-to-reach groups through working with community stakeholders and running campaigns at a local level
- For cervical cancer and prevention in England to be considered for inclusion in the Be Clear on Cancer campaign
- Encourage GP’s to remind patients to book a screening if overdue, either at a face-to-face appointment or by proactively calling non-attenders
- Work alongside companies and employers to educate staff on cervical cancer and encourage working women to take time to attend a screening.
To read the full report click here.
About the report
Demos surveyed 182 cervical cancer sufferers in April 2014. Demos analysis on the savings to the NHS is calculated using figures across just England. However, the benefits of diagnosing and treating cervical cancer at an earlier stage would result in comparable cost savings to health authorities outside England as well.
