There are no products in your shopping cart.
| 0 Items | £0.00 |
If you have questions or need to talk, call our helpline for information or support.
Have a question? Receive a confidential response via email.
Come to a support event to meet other people who have had a cervical cancer diagnosis.
Connect with others, share experiences and ask questions on our forum.
Individual support via phone or email, for anyone affected by a cervical cancer diagnosis.
Read about ways to cope with any effects of treatment and getting practical support.
January 2024 — Please be aware that as of December 2023, the screening programme in Northern Ireland has switched to using HPV primary screening. This page is currently undergoing review, but the information below regarding England, Scotland and Wales remains valid.
HPV primary screening is a way of testing the sample of cells taken at your cervical screening (smear test) appointment. It tests for a virus called high-risk human papillomavirus (HPV) that can cause cervical cell changes to develop into cervical cancer.
We also have information about:
HPV primary screening is used in England, Scotland and Wales. In the future, it will be used in Northern Ireland but the start date is to be confirmed.
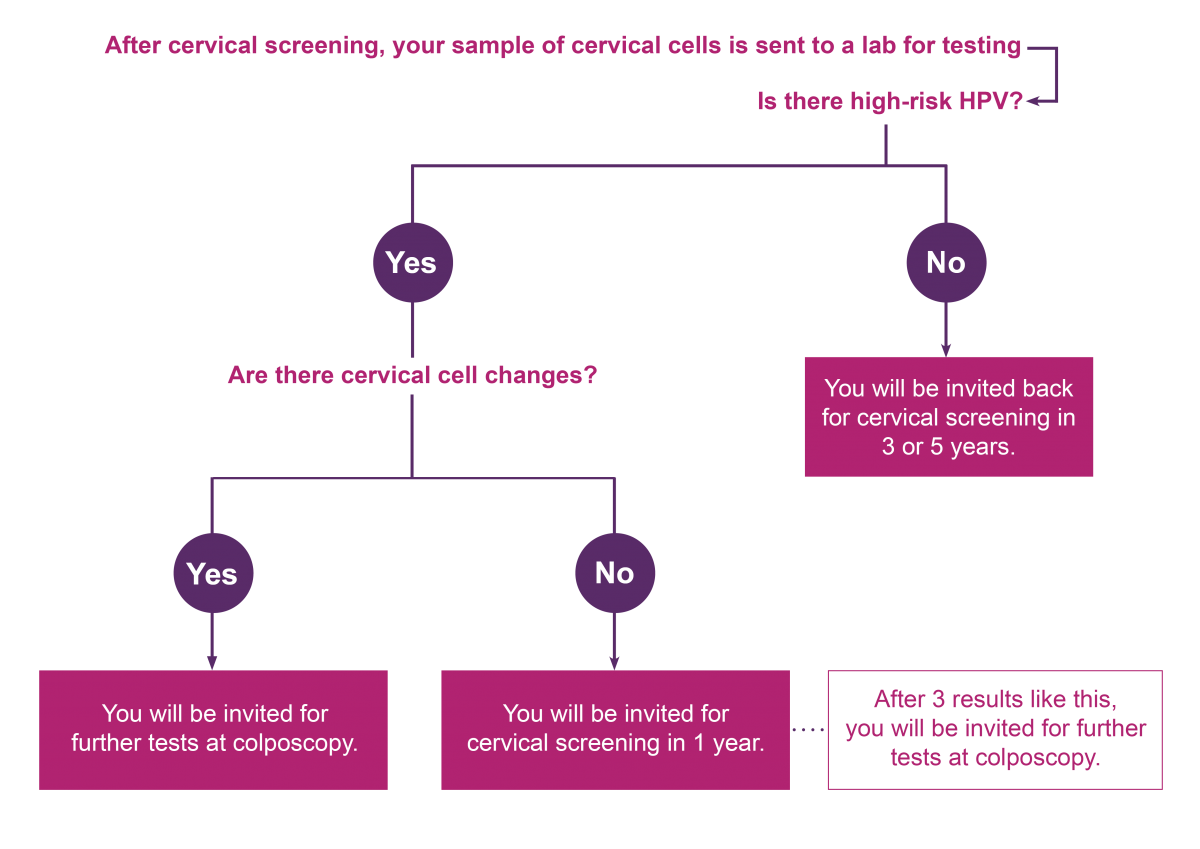
HPV primary screening is a way of testing the sample of cells taken during cervical screening. A lab tests your sample for a virus called high-risk HPV. High-risk HPV can cause cervical cell changes to develop into cervical cancer over time. If you have high-risk HPV, that same sample will be tested for cell changes.
The next steps are based on your result and tailored to your individual risk. You may:
Read about cervical screening results >
If you do not have high-risk HPV, your sample will not be looked at for cell changes. It is very unlikely you will develop cell changes or cervical cancer without having high-risk HPV.
You will be invited for cervical screening in 3 or 5 years, depending on your age and where in the UK you live.
If high-risk HPV is found, your sample will be looked at for cell changes. If there are no cell changes, you will be invited back for cervical screening in 1 year. This is to make sure the HPV has cleared.
If high-risk HPV and cell changes are found, you will be invited for further tests at colposcopy. Not all cell changes develop into cervical cancer, but it is important that they are monitored and treated if needed.
The National Screening Committee, which oversees all screening programmes in the UK, recommended the move to HPV primary screening because evidence shows it is a better test:
All tests have some risks:
Cytology is now only used in Northern Ireland. It is the study of individual cells in the body. In cervical screening, this means that the cells taken during your appointment are looked at under a microscope for changes.
Read more about cell changes >
If you do not have cell changes, your risk of developing cervical cancer is low. You will be invited back for cervical screening in 3 or 5 years, depending on your age.
If you have borderline or low-grade cell changes, the same sample is tested for high-risk HPV. This is called HPV triage.
If you also have high-risk HPV, you will be invited for more tests at colposcopy.
If you have high-grade cell changes, you will be invited for more tests at colposcopy.
It is possible to have cervical cell changes without having high-risk HPV. However, it is unlikely that these cell changes would develop into cervical cancer. The National Screening Committee recommended the move to HPV primary screening because it is more accurate at showing who is at higher risk of cell changes that may develop into cervical cancer.
No, this is not an option. HPV primary screening means your sample will only be tested for cell changes if you have high-risk HPV.
The only way to have your sample checked for cell changes is to book cervical screening privately, for a cost. If you are worried about cervical screening not checking for cell changes, it is best to speak with your GP or practice nurse. They will be able to answer any questions and offer reassurance.
If you live in England, Scotland or Wales, your cervical screening test will be HPV primary screening. Northern Ireland will switch to HPV primary screening in the future.
This is extremely rare. Scientists have known since the 1990s that nearly all cervical cancers are caused by HPV .
There may be some very rare types of cervical cancers that develop without HPV. There can also be problems with some types of testing in the past that missed the HPV.
Even though this is extremely rare, it’s important to be aware of any symptoms and changes and to contact your GP if you are worried.
Before 2019 in the UK HPV testing was not widely used. It’s likely that some women were diagnosed with cervical cancer, but they did not know that this was caused by HPV.
Your GP or practice nurse should be able to answer any questions you have about HPV primary screening and your results.
We know that HPV and HPV primary screening can be confusing, so if you have questions we are also here to support you:
Thank you to all the experts who checked the accuracy of this information, and the volunteers who shared their personal experience to help us develop it.
We write our information based on literature searches and expert review. For more information about the references we used, please contact [email protected]
Understand what HPV is and how it is linked to cell changes and cervical cancer.

If you have questions or need to talk, call our helpline for information or support.

