There are no products in your shopping cart.
| 0 Items | £0.00 |
If you have questions or need to talk, call our helpline for information or support.
Have a question? Receive a confidential response via email.
Come to a support event to meet other people who have had a cervical cancer diagnosis.
Connect with others, share experiences and ask questions on our forum.
Individual support via phone or email, for anyone affected by a cervical cancer diagnosis.
Read about ways to cope with any effects of treatment and getting practical support.
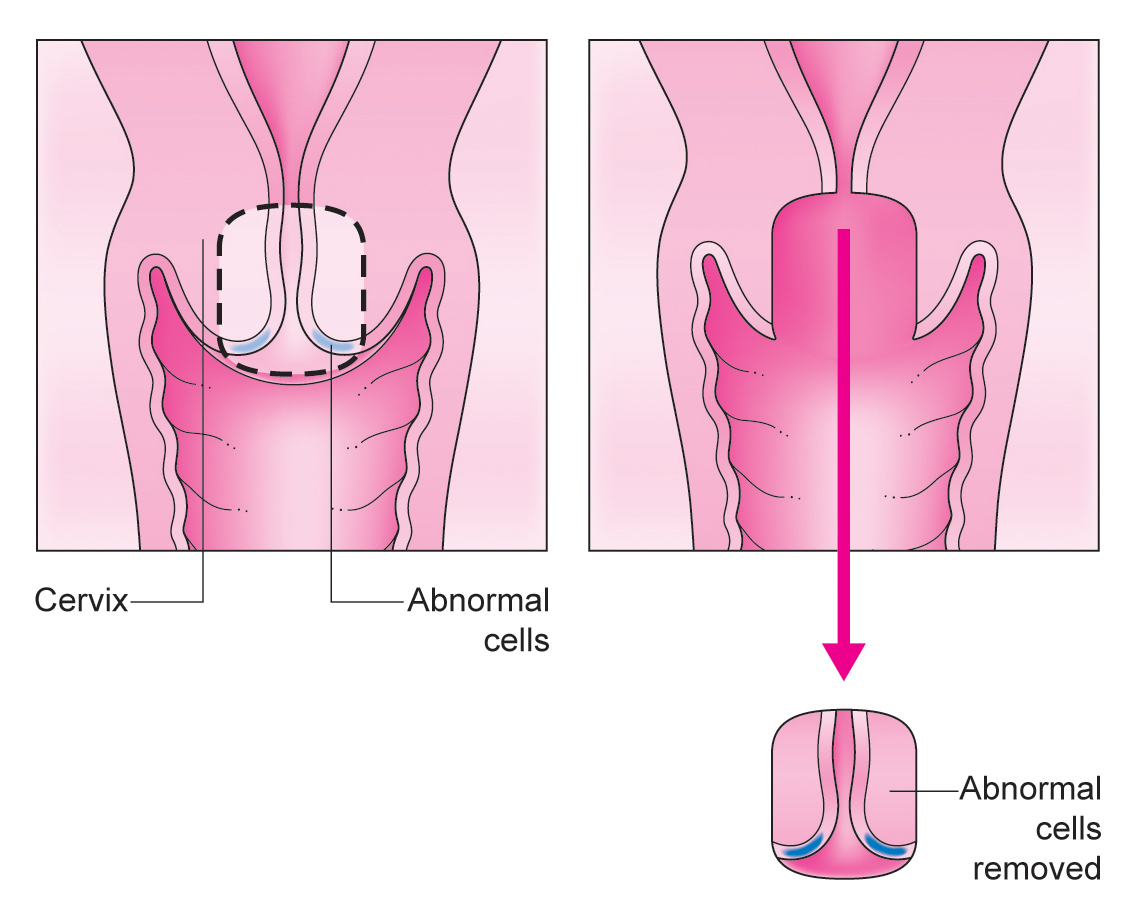
A cone biopsy is a type of surgery that removes a cone-shaped piece of tissue from your cervix. It can be used treat cervical cell changes (abnormal cells) or early stage cervical cancer, as well as to diagnose cervical cancer.
This information is written for people having a cone biopsy for cervical cell changes or cervical cancer. We know that having surgery can be overwhelming, so we hope this page helps you feel prepared. If you need more support, remember that we are here for you in other ways too. You could give us a call on 0808 802 8000 or use one of our other support services.
On this page:
The nature of gynaecological and obstetric care means that intimate examinations are often necessary. We understand that for some people, particularly those who may have anxiety or who have experienced trauma, physical abuse or sexual violence, such examinations can be very difficult. If you feel uncomfortable, anxious or distressed at any time before, during, or after an examination, please let your healthcare professionals know. If you find this difficult to talk about, you may communicate your feelings in writing.
Your healthcare professionals are there to help and they can offer alternative options and support for you. Remember that you can always ask them to stop at any time and that you are entitled to ask for a chaperone to be present. You can also ask to bring a friend or relative if you wish.
If you find intimate examinations difficult, we are here to support you. You can speak with our volunteers on 0808 802 8000 or you may prefer to contact us online.
Before you make a decision about treatment, it is important to understand the procedure, including benefits, risks and possible effects. Your colposcopist should explain these to you and give you the chance to ask any questions. You may also want to talk over your options with your family or friends.
It can help to write a list of questions and take it to your appointment. The form below suggests some questions you might like to ask and has space for you to write down any others you think of.
A cone biopsy is a small surgery. It removes a cone-shaped piece of tissue from the cervix.
You might be offered a cone biopsy if:
Your appointment will happen in a colposcopy clinic at a hospital. You may have a cone biopsy as an outpatient or an inpatient. This could mean you either:
You usually have a general anaesthetic for a cone biopsy. This means you will be asleep during the surgery and won’t feel anything.
The hospital wants to keep you and their staff protected from COVID-19 (coronavirus), so they will be following government guidance on social distancing and using appropriate personal protective equipment (PPE), including masks, gloves and aprons. You will also need to wear a face covering while in the hospital.
If you take blood thinning medication or have a condition that affects your blood, it is important to tell your colposcopist before your appointment. You may have a higher risk of bleeding after the treatment.
A cone biopsy is done under general anaesthetic, which means you are asleep and won’t feel anything. The treatment takes about 15 minutes. Afterwards, you may have to stay in hospital overnight.
A cone biopsy can be done with a:
After a cone biopsy, your doctor may put a small pack of gauze (like a tampon) in your vagina to stop bleeding. You may also have a tube (a catheter) to drain urine from the bladder while the gauze pack is in place. The gauze and tube are usually removed within 8 hours. Once they have been removed, you can go home.
A cone biopsy is usually done under general anaesthetic. This means you will be asleep during the surgery and won’t feel anything.
Cone biopsies are occasionally done under local anaesthetic if a very small area needs to be removed. This is where the part of your body is numbed so you can’t feel anything, but you are still awake.
Some people feel worried about having a general anaesthetic. If you feel this way, you could speak to your healthcare team and anaesthetist before, to find more about what will happen and talk through any concerns. You can also speak to your healthcare team about which type of anaesthetic you would prefer.
When it’s time to have the surgery, you will be taken to a room next door to the operating theatre in a hospital bed. An anaesthetist will give you injections – one to make you fall asleep and one to make your body numb. Once you are asleep, you will be wheeled into the operating room.
The anaesthetist will ask you to count to 10 and before you reach 7, you will drift off to sleep. You will wake up in the recovery room, once the surgery is done.
A cone biopsy is done vaginally, like cervical screening and colposcopy.
Your surgeon will use a speculum (plastic tube) to open your vagina. They will then remove a small, cone-shaped piece of tissue from your cervix. It is usually about 1cm wide.
A cone biopsy is normally done with a scalpel. This is known as a surgical knife or cold knife cone biopsy.
After your surgeon has removed the tissue, they will place some gauze inside your vagina to stop any bleeding. This is called a vaginal pack and looks a bit like a large tampon or rolled-up bandage.
You might also have a thin tube put into your bladder. It might be done through the tube you wee from (urethra) or a small opening in your lower stomach. The catheter helps to drain your wee. It can be removed once the vaginal pack is removed.
Read about catheters on the NHS website >
The tissue that was removed will be sent to laboratory. A specialist called a histopathologist will look at it under a microscope. They will check whether all the cell changes or cancer cells have been removed.
You should get these results within 4 to 8 weeks. You can ask your healthcare team exactly how long you will have to wait.
After the operation, you go back to the outpatient clinic or a ward to recover.
A nurse will make sure you are recovering from the general anaesthetic by checking your:
They will also check that the vaginal pack is in place and for any bleeding.
You may be able to go home the same day. You usually need to be in hospital for about 6 hours so the general anaesthetic can wear off. In some cases, you might need to stay in hospital overnight or longer if your healthcare team want to do more checks.
Your healthcare team will usually take the pack out of your vagina, and remove the catheter within 24 hours after your cone biopsy. You may be monitored once the pack is removed, to check there is no heavy bleeding.
You will not be able to drive, so it is important to arrange transport home. This might be a friend or family member, or public transport.
Once you are home, it usually takes between 1 to 2 weeks to recover from a cone biopsy, although side effects can last longer.
You may have some physical effects after cone biopsy. These usually last up to 4 weeks. Until these have stopped, it is best to avoid:
If you have any questions about what you can and can’t do after cone biopsy, speak with your colposcopist.
If all the cell changes have been removed and there are no cancer cells, you will be invited for a follow-up appointment at the hospital in 6 months. At this appointment, you will have cervical screening (a smear test). This tests for high-risk human papillomavirus (HPV) that causes almost all cervical cancer.
If you don’t have high-risk HPV, you will be invited back for a follow-up appointment every year for 10 years. You will continue to have cervical screening at these appointments.
If you result shows you have high-risk HPV, the same sample will be tested for cell changes:
Cone biopsy is usually successful. The benefit of the treatment is that it can prevent potential cervical cancer from developing or remove cervical cancer which, in many cases, will outweigh the risks. However, like all treatments, cone biopsy has risks and you may have some physical or emotional effects because of the treatment.
Talk to your colposcopist before treatment if you are worried about any risks. They can answer your questions and give you support. After treatment, your GP or a specialist doctor will be able to offer support.
About 85 in 100 (85%) people experience bleeding after this type of treatment. About 15 in 100 (15%) people do not experience bleeding. Bleeding is expected after cone biopsy and can last between 2 days to up to 4 weeks.
You may have bleeding because of the soft scab that forms on the cervix where the cells were removed. This may bleed while it heals.
The bleeding is usually like a period, but may be slightly heavier than your normal period. About 10 days after treatment, the bleeding may get heavier. This is common and a sign that the scab is healing. Your first period after treatment may be slightly heavier or out-of-sync with your regular cycle.
Important! If you are on blood thinning medication or you have a haematological condition, you must tell your colposcopist because you may have a higher risk of bleeding after cone biopsy. If the bleeding is soaking through a period pad every hour, call the contact number given by your colposcopy team or call 111 out of hours. This is sometimes called delayed haemorrhaging. The hospital team or 111 will be able to advise you and make sure you get the right care.
About 67 in 100 (67%) people experience pain after this type of treatment. About 33 in 100 (33%) people do not experience pain.
Some pain is expected for between 2 days to up to 4 weeks after treatment. The pain varies from person to person, but should not be too severe. It is often described as a cramping pain, like a period. You can talk to your doctor about over-the-counter medication that should help.
Important! Some people may experience pain for longer, but it usually goes away within 3 months. If you are in a lot of pain or find it is affecting your day-to-day life, talk to your GP. They can advise on pain medication, offer reassurance based on your medical history and, if needed, will be able to check you are healing properly.
About 65 in 100 (65%) people have changes to their vaginal discharge. About 35 in 100 (35%) people don’t have any changes to their vaginal discharge.
Changes to vaginal discharge can last for about 4 weeks. Straight after treatment, you may have a watery, brown vaginal discharge.
About 10 days after treatment, you may notice a coffee granule-like vaginal discharge. This is normal and a sign that the soft scab on your cervix is healing.
Important! Between about 1 and 14 in 100 (0.8% to 14%) people get an infection after cone biopsy. Talk to your GP if your vaginal discharge smells bad, or is a yellow or green colour. If there is a chance you have an infection, you will be offered antibiotics.
You should still be able to have children after a cone biopsy. It’s a smaller surgery, so you will still have:
After a cone biopsy there is a slightly higher risk of miscarriage and premature birth, as well as complications if the baby is very premature. This can be very distressing to think about.
If you have had a cone biopsy, the risk of giving birth before 37 weeks is about 11 in 100 (11%). If you have not had treatment, this risk is about 7 out of 100 (7%).
If you get pregnant in future, it is important to tell your midwife that you have had a cone biopsy. They may offer to do an ultrasound scan of your cervix. If they think it is short and there is a risk you may have the baby a bit early, they may offer you a cervical stitch (cervical cerclage). This is an operation where a stitch is placed around the cervix. It is usually done between 12 and 24 weeks of pregnancy, although it may be done later.
Speak to your healthcare team to find out your individual risks and what can help. The charity Tommy’s also provides information about having a safe and healthy pregnancy.
Read about pregnancy on the Tommy’s website >
Jo’s Cervical Cancer Trust has spoken with women and people with a cervix who have had treatment for cervical cell changes to understand their experiences. In most cases, they had LLETZ for high-grade cell changes – CIN2 or CIN3. The figures in this section are taken from that research to help you feel as prepared as possible.
It is important to remember that everyone heals at a different pace and will have a different experience after treatment.
You may have strong feelings about what treatment means for your physical wellbeing and future. These feelings could be positive, such as relief that you have had treatment, but you may also feel worried about how your body will recover.
For the women and other people with a cervix that we spoke with:
All of your feelings and concerns, including any we don’t mention in this guide, are valid and it is important you get the right support to deal with them. Here are some of the ways you could get support.
Some people find that a support network of friends and family helps their emotional recovery after treatment. There are lots of ways they can help, from talking your feelings through, to offering a distraction and positive presence.
Before, during and after treatment, you will be in the care of professionals who want to make the experience as good as possible for you. If you are worried about anything, talk to them so they can give you the right support and ease any concerns. Or, if you have another doctor you know and trust, ask to talk with them about any worries.
There are many charities and organisations who offer support services so you can feel listened to and work through your feelings. These services can also signpost to other places that may be able to help.
If you feel that expert support would help, you can self-refer or ask your GP to make a referral for NHS counselling. You can also make an appointment privately, for a cost.
You may experience sex and intimacy differently after treatment. This may also have an impact on your relationships. These differences may be because of physical changes, emotional changes, or both.
In the women and other people with a cervix that we spoke with, about 46 in 100 (46%) had changes to how they feel, while 54 in 100 (56%) did not. These changes included feeling less attractive or confident, as well as worries about passing on HPV.
About 33 in 100 (33%) people had pain during or after sex, while 67 in 100 (67%) did not. In most cases, this pain lasted for less than 3 months. In some cases, pain during or after sex lasted for:
About 22 in 100 (22%) people had bleeding during or after sex, while 78 in 100 (78%) did not. In most cases, the bleeding lasted for less than 3 months. In some cases, the bleeding lasted for:
It is important to see your GP if you have any symptoms such as pain or bleeding. They can examine you and talk through ways to make it better, such as using more lubricant during sex to lessen any pain.
It may help to speak to a trusted person about any loss of confidence – whether that is a partner, family, friends, your GP, or other people who have had treatment. Talking through your worries might ease them or give you new ideas about how to handle them.
If you and a partner are struggling to reconnect after treatment, you may want to consider couples counselling. An unbiased expert can help you start and explore conversations around sex and intimacy, so you can find solutions together. You can self-refer through local NHS services, speak with your GP, or search for a local counsellor yourself.
We understand that waiting for or having a cone biopsy can be stressful, but you don’t have to cope with any emotions alone. Talking to your colposcopy team is a good place to start and we are also here to support you.
If you need some extra support, you can give our free Helpline a call on 0808 802 8000. Our trained volunteers can talk through the different pathways or simply listen to how you’re feeling.
Sometimes connecting with others who have gone through a similar experience can be helpful. Our online Forum lets our community give and get support. You can read through the messages or post your own – whichever feels most comfortable.


We want to see a future free from cervical cancer. By making a regular gift you could help us get closer to that day.

